Short-term complications favor Mohs
With Todd E. Schlesinger, MD

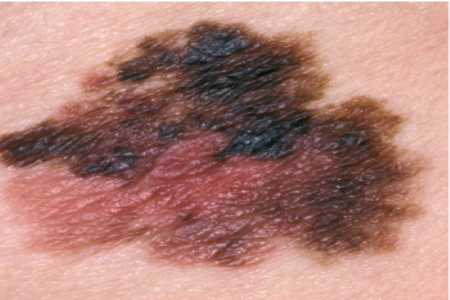
Dermatologists are always looking for the safest, most effective treatments for skin cancers such as melanoma in situ (MIS). According to a study presented at the American Academy of Dermatology VMX, Mohs micrographic surgery (MMS) might provide a better short-term side effect profile than the current standard, wide local excision (WLE).1
Regarding overall survival and recurrence rates, prior research has shown that MMS may provide results equivalent to those of WLE for MIS.2,3 However, we do not know whether WLE or MMS leads to a higher risk of negative short-term outcomes.
To answer this question, the authors performed a retrospective cohort study using TriNetx, a real-time international database including 61 million patient records from 2006 to 2020. Using current procedural terminology (CPT) and international classification of diseases, tenth revision, clinical modification (ICD-10) codes, they calculated adjusted risk ratios (ARRs) for 30-day complications associated with MMS and WLE for MIS.
A matched cohort of 9390 patients revealed that the MMS group experienced significantly lower rates of 4 sequelae in particular:
- Cellulitis/lymphangitis (ARR 0.38; 95% confidence interval/CI, 0.24-0.61)
- Cutaneous infection (ARR = 0.52; 95% CI, 0.39-0.69)
- Wound dehiscence (ARR = 0.48; 95% CI, 0.27-0.84)
- Hematoma (ARR = 0.44; 95% CI, 0.21-0.91)
Rates of other postsurgical complications such as pain, pruritus, and hypertrophic scarring were similar between the 2 treatments.
“The key take-home of this study is that Mohs surgery should be considered a viable option for treating MIS even though the current standard of care is wide local excision,” lead author Rahul Raiker, BS, told The Dermatology Digest. He is a medical student at West Virginia University School of Medicine.
Given the rise in melanoma rates in recent years, dermatologists may consider shifting to Mohs surgery for MIS as it provides a similar cure rate while being cost-comparable,4 noted co-author Haig Pakhchanian, BS. He is a medical student at George Washington University School of Medicine and Health Science.
“However,” added Mr. Raiker, “Mohs is a much more time-consuming and involved procedure than wide local excision, and this is why Mohs has not been widely adopted for MIS.”
The study is interesting because in some cases, MMS may produce a smaller defect than WLE. It makes sense that the complication rate might be lower, adding validity to what we might expect, provided we are confident that MMS can achieve a consistent clear margin. Additionally, MMS might permit a wider variety of closure options because knowing that the margins are clear allows for more creative closure techniques.
Dermatologists may wish to consider the size of the defect that may result from removing MIS by WLE, particularly when the tumor is in an area in which WLE may create a defect that is difficult to close without excessive tension, or where the skin quality might not be optimal. These factors increase complication rates, and MMS may add value in such situations.
Study strengths include its large, national sample size, with data from multiple centers, and the robust statistical methods used. As a retrospective study, authors allow, data reporting could be subject to bias and coding errors.
Going forward, Raiker and colleagues call for additional studies—especially subgroup comparisons of MIS in different body locations—to validate their findings. Assessing complication severity could also be an avenue for future studies, Mr. Raiker said.
Additionally, future research perhaps could compare defect sizes between cohorts to see if MMS closures were indeed smaller or under less tension. This would help us understand if it was the MMS itself that resulted in the difference we see, or if it was simply related to closure dimensions.
REFERENCES
1. Raiker R, Pakhchanian H, Patel VA. Short-term complications of Mohs surgery versus wide local excision in patients with melanoma in-situ. Poster 26749. American Academy of Dermatology VMX; April 23-25, 2021.
2. Nosrati A, Berliner JG, Goel S, et al. Outcomes of melanoma in situ treated with Mohs micrographic surgery compared with wide local excision. JAMA Dermatol. 2017;153(5):436-441.
3. Phan K, Loya A. Mohs micrographic surgery versus wide local excision for melanoma in situ: analysis of a nationwide database. Int J Dermatol. 2019;58(6):697-702.
4. Bialy TL, Whalen J, Veledar E, et al. Mohs micrographic surgery vs traditional surgical excision: a cost comparison analysis. Arch Dermatol. 2004;140(6):736-742.
DISCLOSURES
Dr. Schlesinger, Mr. Raiker, and Mr. Pakhchanian report no relevant financial interests.