A Dying Penis
With Ted Rosen, MD, FAAD
CASE HISTORY
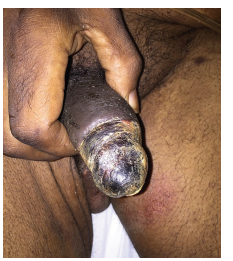
A 45-year-old Black male with poorly controlled Type 1 diabetes and chronic renal disease presented to the Emergency Department with a three-week history of a gradually expanding and extremely painful penile lesion.
On the visual analog scale (VAS), his pain was assessed to be 9 out of 10. Aside from routine hemodialysis, the patient denied any recent medical procedures or instrumentation. A battery of tests was ordered, including a rapid plasma reagin (RPR), HSV-2 and HIV serologies, a CBC and complete metabolic panel, clotting studies, and an antinuclear antibody (ANA) and rheumatoid factor. The patient was appointed to see Urology Service and Dermatology the following day and was given oral cephalexin for presumed infection and opioid narcotics for pain.
On presentation the next day, the patient was diaphoretic due to discomfort but afebrile. He had a necrotic eschar covering virtually all of the glans penis and extending cephalad to involve the corona, the coronal sulcus and the distal penile shaft.
Laboratory values obtained in the ED the previous day were negative or normal except: elevated calcium-phosphate product of 58 mg/dL (upper limits of normal 52.5), blood glucose of 212 mg/dL, creatinine of 3.4mg/dL and BUN of 48mg/dL. A plain abdominopelvic film was unrevealing. A CT scan (done without contrast) showed calcification in the internal iliac and internal pudendal arteries. The patient was admitted for further workup and treatment.
What does the patient have and what is his prognosis?
DISCUSSION
A small skin biopsy done just proximal to the edge of the eschar showed intraluminal calcium deposits within arterioles and prominent hyperplasia of the intima and media. Considering the underlying chronic renal disease and diabetes, the elevated calcium-phosphate product, the imaging results and the overall clinical picture, a diagnosis of penile calciphylaxis was made.
Although intravenous sodium thiosulfate, the drug of choice, was started almost immediately, the necrosis continued to progress and pain was essentially refractory to medical management. Therefore, a partial penectomy was performed. The patient stabilized and survived.
Calciphylaxis is a rare phenomenon, affecting about 1% of those with chronic renal insufficiency, especially those with diabetes as an etiology of the chronic kidney disease. Penile involvement is seen in only about 6% of all calciphylaxis cases, likely due to extensive collateral circulation protecting the male genitalia from ischemia. Penile calciphylaxis carries a grave prognosis: 50% to 65% mortality within 2.5 to 6.0 months despite medical or surgical intervention. Diagnosis is usually based on the constellation of clinical signs and symptoms in a patient at high risk due to underlying comorbidities. There is no specific diagnostic test. Imaging demonstrating extensive calcification in the blood vessels supplying the necrotic skin region is supportive of the diagnosis, but not necessary. Administration of warfarin, steroids, and vitamin D preparations may facilitate the development of calciphylaxis.
Therapy for penile calciphylaxis consists of intravenous sodium thiosulfate and debridement of necrotic tissue, along with meticulous metabolic support. Hyperparathyroidism may be present and should be treated with parathyroidectomy, although the survival rate is not statistically improved in some studies. Penectomy may be required for progressive disease, as in this case.