Douglas Laux, MD, with John Jesitus
Patients with Merkel cell carcinoma (MCC) and cutaneous squamous cell carcinoma (cSCC) refractory to programmed cell death protein 1 (PD-1) inhibition may one day have a silver bullet that renders these cancers susceptible to PD-1 checkpoint inhibitors. This is one of the goals for the clinical development of cavrotolimod (also called AST-008, Exicure), a novel toll-like receptor 9 (TLR9) agonist that is currently the focus of an ongoing phase 2 clinical trial for these indications.
Patients with MCC or cSCC who have never responded to or who have lost response to PD-1 inhibition have limited subsequent options, said Douglas Laux, MD. “So we’re looking for a way to sensitize or in some cases re-sensitize this disease to immune checkpoint inhibitor therapy.”
TLR9 agonists, which naturally include bacterial and viral DNA oligonucleotides that are rich in unmethylated CpG repeats, can shift the immune environment to a pro-inflammatory interferon-1-like milieu. Such an environment attracts and activates T cells and natural killer (NK) cells, both of which offer antitumor effects. “Cavrotolimod helps to recruit these cells into the tumor microenvironment and to activate them, harnessing the power of both the innate and adaptive immune responses against the cancer,” said Dr. Laux.
Compared to linear oligonucleotide TLR9 agonists, cavrotolimod leverages Exicure’s proprietary spherical nucleic acid (SNA) technology, Dr. Laux said. SNAs have a strong affinity for scavenger receptors on the surfaces of cells, which leads to high cellular uptake in the compartment containing TLR9. Targeting TLR9, which is expressed mainly on dendritic cells and B-cells, leads to a cascade of innate and adaptive immune responses against the tumor. SNAs consist of a benign lipid nanoparticle core, from which strand-like oligonucleotides radiate.1 The dense spherical arrangement of these oligonucleotides and high cellular uptake ultimately lead to enhanced stimulation of TLR9, resulting in more efficient and potent activation of this receptor.
Trial observations
In the phase 1b dose-escalation portion of the ongoing phase 1b/2 trial, investigators treated 20 patients with inoperable advanced or metastatic solid tumors—mostly melanoma and MCC—using cavrotolimod combined with intravenous pembrolizumab. Patients underwent intratumoral (IT) cavrotolimod injections once weekly for 8 weeks, then once every 3 weeks; pembrolizumab dosing occurred every 3 weeks, starting at week 3.
As of November 2020, interim results of the phase 1b stage demonstrated a confirmed overall response rate (ORR) of 21%.1,2 This figure includes one complete response and 3 partial responses, which investigators defined as at least 30% tumor shrinkage from baseline. Among the 4 responders, 3 had actively progressing disease on PD-1 blockade at study enrollment. “This helps to support the concept that by giving cavrotolimod with a PD-1 inhibitor, we can help to re-induce tumor response to immune checkpoint inhibitor therapy,” said Dr. Laux.
At the highest dose, 32 mg, ORR was 33%. Of 6 patients given this dose, 2, both with melanoma, responded. Two patients with MCC responded to doses of 2 mg and 4 mg, respectively. As of November 2020, progression-free survival exceeded 6 months in all 4 responders, and 16 months in 2 of them.
Additionally, investigators observed shrinkage of noninjected tumors distant from the injection site, demonstrating an abscopal response. For example, one patient with cSCC experienced not only 33% reduction of an injected facial tumor, but also reductions in neck and lung tumors of 33% and 20%, respectively.
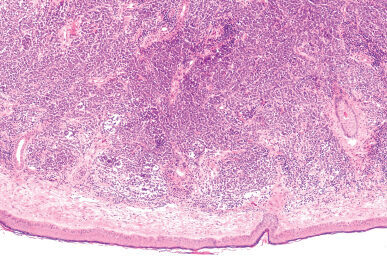
“The idea is that by injecting cavrotolimod directly into a tumor, we’re not only changing the immune environment to a pro-inflammatory phenotype in and around that lesion, but we’re also stimulating antigen presenting cells and B cells to activate effector NK cells and CD8+ cytotoxic killer T cells to recognize and kill tumor cells at other sites,” said Dr. Laux. Increased serum interferon gamma-induced protein (IP)-10 levels observed in responders attest to this systemic effect. Likewise, preliminary immunohistochemistry data from the injected tumor of one responder reflect increased levels of infiltrating CD45RO+ memory T cells.1
Flu-like side effects, which investigators expected, also support the presence of a systemic immune response, he said. Low-grade flu-like symptoms and injection-site reactions were the most common adverse events (AEs), occurring in all patients at the highest dose; 98% of treatment-related AEs were grade 1 or 2. In the phase 1b stage, 2 patients reported treatment-related grade 3 AEs, which were injection-site reactions and psychological agitation.
The phase 1b trial demonstrated promising pharmacodynamic potential for combination treatment with cavrotolimod, as well as strong safety data and evidence of systemic, abscopal responses. Said Dr. Laux, “We now have early evidence that this is a worthwhile strategy to pursue for patients who have PD-1 refractory disease. We’re excited to be able to move on to phase 2 (NCT03684785) in patients with PD-1 refractory Merkel cell carcinoma and cutaneous squamous cell carcinoma.”
Ongoing research
Including Dr. Laux’s site at the University of Iowa, researchers at 16 sites have begun enrolling patients with such cancers. Each cohort of up to 29 patients will receive the 32 mg dose of cavrotolimod, combined with the PD-1 inhibitor pembrolizumab (MCC) or cemiplimab (cSCC).3 The first patient in the MCC cohort was dosed in June 2020.
The trial also will include exploratory cohorts to evaluate cavrotolimod administered in a subcutaneous fashion, as well as given as an injection into liver metastases in combination with pembrolizumab in patients with locally advanced or metastatic PD-1 refractory solid tumors without superficial lesions.4
In January, the FDA granted fast-track designation to cavrotolimod for PD-1 refractory MCC and cSCC. Regarding how soon cavrotolimod could become available if the clinical development and approval process goes well, Dr. Laux said it is too soon to speculate. “At this time, we are focused on enrollment on the phase 2 portion of the trial and are looking forward to evaluating the data from this study.”
References
1. O’Day SJ, Perez CA, Wise-Draper T, et al. Safety and preliminary efficacy of intratumoral cavrotolimod (AST-008), a spherical nucleic acid TLR9 agonist, in combination with pembrolizumab in patients with advanced solid tumors. Abstract 423. Society for Immunotherapy of Cancer Annual Meeting. November 9-14, 2020.
2. Milhem MM, Perez CA, Hanna GJ, et al. Phase 1b/2 studying of an intratumoral TLR9 agonist spherical nucleic acid (AST-008) and pembrolizumab: evidence of immune activation. Abstract LB-140.American Association for Cancer Research Virtual Annual Meeting. June 22-24, 2020.
3. Milhem MM, Perez CA, Hanna GJ, et al. AST-008: a novel approach to TLR9 agonism with PD-1 blockade for anti-PD-1 refractory Merkel cell carcinoma (MCC) and cutaneous squamous cell carcinoma (cSCC). J Clin Oncol. 2020 May; 38(15_suppl):TPS3164.
4. Intratumoral cavrotolimod combined with pembrolizumab or cemiplimab in patients with Merkel cell carcinoma, cutaneous squamous cell carcinoma, or other advanced solid tumors. ClinicalTrials.gov identifier: NCT03684785. Updated January 12, 2021. Accessed March 5, 2021. https://www.clinicaltrials.gov/ct2/show/NCT03684785
Disclosures
Dr. Laux reports no relevant financial interests.