Cutibacterium acnes significantly influences the bacterial community in hypopigmented Lichen striatus (LS), new research shows.
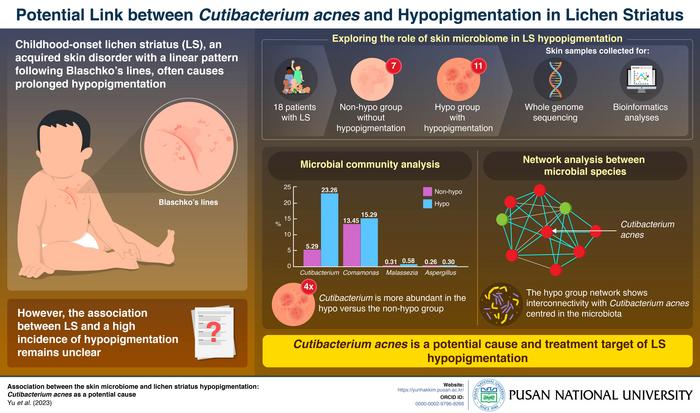
For the study, researchers from Korea led by Associate Professor Yun Hak Kim from the Department of Anatomy and the Department of Biomedical Informatics and Professor Hyun-Chang Go from the Department of Dermatology, both at Pusan National University, analyzed skin samples of 18 patients with LS (11 with hypopigmentation and 7 without it) confirmed by biopsy through whole genome sequencing and performed bioinformatics analyses to assess microbial differences in the samples.
Despite the diverse stages of LS in patients with hypopigmentation, significant differences were observed in their skin microbiomes. This observation suggested a strong association between LS hypopigmentation and the skin microbiome. Comparing patients with LS with and without hypopigmentation, the researchers discovered a quadrupled presence (23.26% versus 5.29% of the entire microbiota) of Cutibacterium acnes in the former.
“Through network analysis between various microbial species found in the skin samples of patients with LS, we observed that C. acnes significantly influenced the bacterial community in hypopigmented LS, holding a central position in relationships with other bacteria. It further strengthens its potential association with LS hypopigmentation pathogenesis,” says Dr. Kim in a news release.
The research team additionally identified Malassezia, a genus associated with hypopigmentation in other skin disorders, in abundance among patients with LS with hypopigmentation (0.58% versus 0.31% of the entire microbiota). The presence of Malassezia restricta points at a potential link between Malassezia and LS hypopigmentation for targeted future research. In addition, Comamonas (15.29% versus 13.45% of the entire microbiota) and Aspergillus (0.30% versus 0.26% of the entire microbiota) were identified as other likely candidates.
Overall, there is likely a relationship between imbalance in the skin microbiota and LS-associated hypopigmentation. The frequency of Malassezia and C. acnes in hypopigmented LS cases suggests that these two conditions could be novel treatment targets for reducing LS duration as well as hypopigmentation.
Future studies exploring temporal changes in the microbiome and observing the effects of antibiotic or antifungal agents on hypopigmentation frequency and duration could offer insights into causative or correlative relationships between microbiome alterations and LS hypopigmentation.
“Our findings provide promising avenues for further research to decipher the relationship between skin microbiota and LS hypopigmentation, ultimately aiming to elucidate novel therapeutic strategies,” Dr. Kim says.
Their paper was published in the Journal of the European Academy of Dermatology & Venereology.