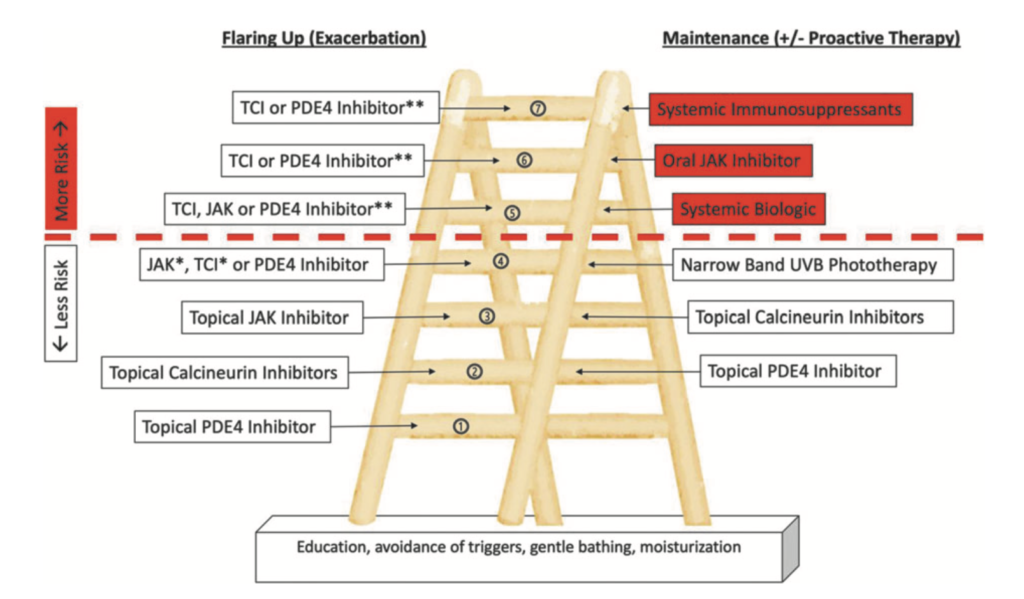
A newly developed therapeutic ladder can help guide dermatologists and patients on the use of nonsteroidal treatment options for atopic dermatitis (AD).
Nonsteroidal treatment options for AD have rapidly expanded in recent years with the development of phosphodiesterase-4 inhibitors, biologics, and Janus kinase (JAK) inhibitors. Although topical corticosteroids are still considered the first line in AD, adverse effects can occur especially with prolonged usage.
The new ladder divides nonsteroidal medication classes into treatments for exacerbations and maintenance therapies in an escalating order based on their increasing potential for adverse effects.
The foundational aspects of AD care –education, gentle bathing, avoiding triggers, and moisturizing — apply to all levels are the base of the ladder, explain study authors Peter Y. Ch’en, a medical student at the Albert Einstein College of Medicine in the Bronx, New York, and Peter A. Lio, MD, a Clinical Assistant Professor of Dermatology and Pediatrics at Northwestern University Feinberg School of Medicine and a partner at Medical Dermatology Associates of Chicago.
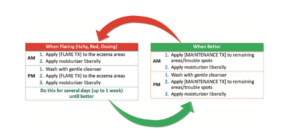
From there, the treatments are ranked in terms of increasing potential for adverse effects. The new topical therapies constitute the lower rungs of the therapeutic ladder and can be used for both exacerbations and maintenance. Rung No. 2 lists topical calcineurin inhibitors (TCIs) on the left and PDE-4 inhibitors on the right. Thus, a TCI would be written into the plan in place of ‘‘[FLARE TX]’’ and a PDE-4 inhibitor would be written into the plan in place of ‘‘[MAINTENANCE TX].
Treatment failure is not required before advancing up the ladder. Other considerations that could warrant skipping a rung or rung of therapy can include patient preference, accessibility, adverse events, and tolerability.
The dotted red line in the ladder represents the boundary between safer therapies and systemic treatments with more significant safety risks.
Before moving to such therapies, dermatologists should confirm the diagnosis of AD via patch testing, scabies preparation, wound culture, or skin biopsy and ensure that maximization of topical therapy has been attempted. Adjunctive approaches such as wet wrap treatments, soaks, and antimicrobial approaches can also included in the ladder.
The study appears in Dermatitis.